Introduction:
Depression is a common internal health issue that affects millions of people worldwide. It’s a mood complaint that can lead to passions of sadness, forlornness, and a loss of interest in conditioning that were formerly pleasurable. While it’s normal to feel down or upset from time to time, depression becomes a cerebral complaint when it interferes with your capability to serve in your diurnal life. In this composition, we’ll explore when depression becomes a cerebral complaint and the signs to look out for.
What is Depression?
Depression is a mental health condition that affects how you feel, think, and act. It’s a mood disorder that can be caused by a variety of factors, including genetics, brain chemistry, and life events. Depression can be mild, moderate, or severe, and the symptoms can last for weeks, months, or even years.
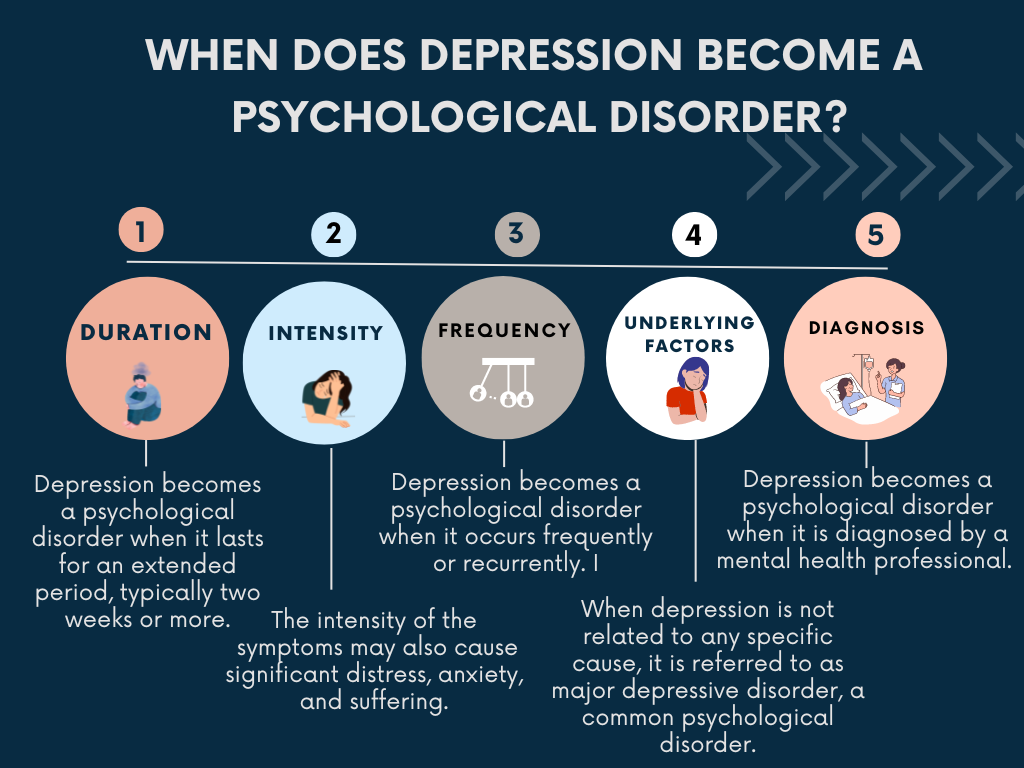
When Does Depression Become a Psychological Disorder?
Depression becomes a psychological disorder when it interferes with your ability to function in your daily life. This means that your symptoms are severe enough to impact your work, school, relationships, and other aspects of your life. Here are some signs that your depression may have become a psychological disorder:
Persistent feelings of sadness, hopelessness, and worthlessness.
Changes in appetite or weight.
Sleep disturbances, such as insomnia or oversleeping.
Fatigue or loss of energy.
Difficulty concentrating or making decisions.
Feelings of guilt or self-blame.
Thoughts of suicide or self-harm.
If you’re experiencing any of these symptoms and they’re interfering with your ability to function in your daily life, it’s important to seek help from a mental health professional.
Types of Depression:
Major Depressive Disorder (MDD): This is the most common type of depression and is characterized by a persistent feeling of sadness and loss of interest in activities that were once enjoyable.
Patient Depressive complaint( PDD) This type of depression is also known as dysthymia and is
characterized by a low mood that lasts for at least two times.
Bipolar Disorder: This is a mood disorder that is characterized by episodes of depression and mania, which is an elevated or irritable mood.
Seasonal Affective Disorder (SAD): This is a type of depression that occurs during the winter months when there is less sunlight.
Causes
Genetic Factors
One of the most important causes of depression is genetic factors. Studies have shown that people who have a family history of depression are more likely to develop this disorder themselves. In fact, research suggests that genetic factors may account for up to 40% of the risk of developing depression.
Several genes have been identified that may contribute to the development of depression, including the serotonin transporter gene, the COMT gene, and the BDNF gene. These genes are involved in the regulation of mood, emotions, and stress, and abnormalities in their functioning may increase the risk of depression.
Biochemical Imbalances
Another significant cause of depression is biochemical imbalances in the brain. Depression is often associated with a reduction in the levels of neurotransmitters such as serotonin, norepinephrine, and dopamine, which are involved in the regulation of mood and emotions.
Low levels of serotonin, in particular, have been linked to depression, as this neurotransmitter is responsible for regulating mood, sleep, appetite, and other important physiological functions. A reduction in serotonin levels can lead to feelings of sadness, anxiety, and irritability, which are common symptoms of depression.
Environmental Factors
Environmental factors can also play a role in the development of depression. Stressful life events, such as the death of a loved one, divorce, financial problems, or job loss, can trigger depression in some people. Traumatic experiences, such as physical or sexual abuse, can also increase the risk of depression.
Chronic stress, such as the stress associated with ongoing health problems, can also contribute to the development of depression. In addition, exposure to toxins, such as heavy metals or pesticides, can affect the functioning of the brain and increase the risk of depression.
Personality Traits
Certain personality traits are also associated with an increased risk of depression. People who are highly sensitive, perfectionistic, or prone to self-criticism are more likely to develop depression than those who are more resilient and adaptable. Similarly, people who have low self-esteem or a negative outlook on life may be more vulnerable to depression.
Other Risk Factors
Substance abuse: Alcohol and drug abuse can lead to depression, both as a result of the direct effects of the substances on the brain and the consequences of addiction, such as social isolation, financial problems, and legal issues.
Chronic illness: People with chronic health conditions, such as diabetes, heart disease, or cancer, are more likely to develop depression, possibly due to the stress and uncertainty associated with managing these conditions.
Lack of social support: People who have few social connections or who feel socially isolated may be more vulnerable to depression.
Treatment for Depression:
Treatment for depression depends on the severity of your symptoms and the type of depression you have.
Psychotherapy: This is a type of talk therapy that can help you identify and change negative thought patterns that contribute to your depression.
Medication: Antidepressant medications can help alleviate symptoms of depression by balancing chemicals in the brain.
Electroconvulsive Therapy (ECT): This is a procedure that uses electrical currents to stimulate the brain and is often used for severe depression that has not responded to other treatments.
Light Therapy: This is a treatment that involves exposure to bright light and is often used to treat seasonal affective disorder.
Conclusion
In conclusion, depression can be a normal and understandable response to life’s challenges and difficulties. However, when it becomes a persistent and pervasive condition that interferes with daily functioning and impairs quality of life, it may be diagnosed as a psychological disorder. The diagnosis of depression as a psychological disorder requires careful assessment by a mental health professional, taking into account the severity, duration, and impact of symptoms on the individual’s overall functioning. Early identification and intervention are critical for successful treatment outcomes. With proper diagnosis and treatment, individuals with depression can recover and lead fulfilling lives. It is important to seek professional help if you or a loved one is experiencing persistent and disruptive symptoms of depression.
FAQS :
What is depression, and how is it different from sadness or grief?
Depression is a mental health condition characterized by persistent feelings of sadness, hopelessness, and despair. It can impact a person’s thoughts, behaviors, and physical health. While sadness and grief are normal human emotions, depression involves a persistent and pervasive sense of sadness that can interfere with daily life.
When does depression become a psychological disorder?
Depression becomes a psychological disorder when it persists for more than two weeks and interferes with a person’s ability to function in their daily life. Symptoms may include feelings of hopelessness, worthlessness, guilt, fatigue, changes in appetite or sleep, and thoughts of self-harm or suicide.
What are the risk factors for depression?
Some common risk factors for depression include a family history of depression, a history of trauma or abuse, chronic stress, and certain medical conditions or medications. Additionally, factors such as social isolation, lack of social support, and substance abuse can increase a person’s risk of developing depression.
How is depression diagnosed?
Depression is typically diagnosed by a mental health professional, such as a psychologist or psychiatrist. They may conduct a clinical interview and use standardized assessment tools to evaluate a person’s symptoms and determine if they meet the diagnostic criteria for depression.
How is depression treated?
Depression is often treated with a combination of medication and psychotherapy. Antidepressant medications can help to alleviate symptoms of depression by regulating brain chemicals that impact mood. Psychotherapy, such as cognitive-behavioral therapy or interpersonal therapy, can help individuals identify and change negative thought patterns and behaviors that contribute to depression. Additionally, self-care strategies such as regular exercise, a healthy diet, and social support can also be helpful in managing depression symptoms.















